Figure 1. Pulse oximetry measures the percentage of hemoglobin (Hb) saturated with oxygen by measuring the absorption of red and IR light passed through a patient's finger (as shown here) or ear lobe. Knowing what percentage of the hemoglobin is saturated with oxygen is important when administering anesthesia or for determining the effectiveness of the respiratory system, as well as for helping diagnose various illnesses.
|
|
Electronic components have been incorporated into medical equipment designs for years. Until recently, medical electronics has been focused primarily on the institutional side of the medical market, in expensive diagnostic equipment, such as MRI and CAT scanning machinery for use in hospitals and clinics. An aging and expanding population is accelerating the development of new and different medical equipment. Professionals in health-care settings want real-time, reliable, and accurate diagnostic results provided by devices that can go to the patient, whether he or she is in a hospital or clinic or at home, being monitored remotely. The equipment should be appropriate for both home care and ambulatory treatment; it must be patient friendly, both technically and physically; and it must be small, light, and energy efficient.
Electronics-based medical equipment requires sensors to convert the various types of stimuli (optical, mechanical, etc.) into electrical form. Many different types of sensors have been included in medical equipment designs. Sensors in current and future medical equipment need to be highly reliable, small, packaged with surface-mount technology (for a smaller footprint on the PCB and for ease of manufacture), low cost, highly accurate, and have no lead content. This article will address why optoelectronic sensors work particularly well in the medical equipment environment, in both institutional and home-care equipment designs.
Optoelectronic Sensor Basics
By definition, an optoelectronic sensor is a device that produces an electrical signal proportional to the amount of light incident on its active area. A number of devices meet this definition, but none is more prevalent than the semiconductor photodiode. Over the years, this two-terminal device has become the mainstay for light sensing.
Designers today—especially medical equipment designers—are now asking for more than just a light-to-current transducer. They are looking for more functionality integrated around this semiconductor workhorse, to provide themselves with improved performance and reliability, and lower system cost in the highly cost-sensitive medical equipment market. Added integrated functionality also removes the need for certain subsystem circuit designs and thus helps shorten the design cycle.
Integrated optoelectronic sensors are designed to respond to light so that they can recognize things such as patterns, images, motion, intensity, and color. The sensor's ability to perform this recognition (and the complexity of the recognition possible) depends upon
|
Figure 2.
|
|
Optoelectronic Sensor Type
|
Description
|
|
Light-to-voltage converters
|
Produce a linear output voltage proportional to light intensity
|
|
Light-to-frequency converters
|
Convert light intensity to digital format for direct connection to a microcontroller or DSP
|
|
Ambient light sensors
|
Measure what the human eye sees
|
|
Linear sensor arrays
|
Measure spatial relationships and light intensity
|
|
Color sensors
|
RGB (red/green/blue) filtered sensors for color discrimination, determination, and measurement
|
|
Reflective light sensors
|
Convert reflective light intensity to a voltage output
|
|
the type of integrated optoelectronic sensor. Some of the basic types of integrated optoelectronic sensors currently in use are outlined in Figure 2.
All of these types of sensors can be, and are, used in medical equipment applications. They help eliminate human error while providing more accurate readings and faster results. Rather than rely on human judgment to match colors or identify changes in light intensity, the sensors are designed to read or measure light— a real-world signal considered to be very stable and highly accurate—in a reliable, repeatable way. Data from the optoelectronic measurements are fed directly into the computer system, removing another possible source of error. The sensors are noncontact, able to perform their sensing or measurement functions without the need for physical contact with specimens such as blood, urine, or other bodily fluids. This is critical because if the specimens are tainted in any way, the resulting readings and measurements may not be accurate.
Current Medical Applications
Current medical applications that use optoelectronic sensors include pulse oximetry, measuring the amount of oxygen in the blood (see "Optical Sensors in Pulse Oximetry"); heart-rate monitors; blood diagnostics, such as blood glucose monitoring; urine analysis; and dental color matching.
Light-to-voltage and light-to-frequency converters serve as the platform on which the other integrated optoelectronic sensors are built, e.g., the IR optoelectronic sensors currently used in pulse oximetry systems and personal heart-rate monitors. These types of optoelectronic sensors integrate other functions such as current-to-voltage conversion, amplification, and A/D conversion, which results in smaller, less costly, and more reliable diagnostic systems. Integrated optoelectronic sensors have helped establish pulse oximetry as a viable medical procedure. Prior to pulse oximetry, medical professionals relied on blood samples to determine blood oxygen content, but these measurements could not give real-time results. Early pulse oximetry systems were large, bulky, and expensive, costing approximately $10,000. With the advent of integrated optoelectronic sensors and better LEDs, modern pulse oximetry systems became possible, enabling real-time, accurate, and noninvasive measurements of blood oxygen content. The use of integrated optoelectronic sensors in personal heart-rate monitors has resulted in similar benefits.
Light-to-voltage and light-to-frequency converters also serve as the platforms for color sensors, which are currently used in blood glucose monitors designed for home use. Blood glucose monitors (see "Integrated Color Sensors in Blood Glucose Meters") presently use one of two different methods:
- The optoelectronic sensor method, in which a drop of blood on a special test strip is read by an optoelectronic sensor, which measures a color change or the reflectance of a particular wavelength of light to determine blood glucose levels.
- The electrochemical method, in which a drop of blood on a special test strip provides an electroresistive measurement to determine glucose levels.
Of the two approaches, the optoelectronic sensor method offers several benefits: The test strips tend to be cheaper to manufacture; testing requires extremely low specimen volumes, leading to less pain for the patient; the method is less sensitive to the presence of prescription and over-the-counter drugs in the patient's system; and compared to the electrochemical method, its accuracy is less affected by the number of red blood cells present.
The accuracy and speedy results enabled by integrated color sensors also make them the optoelectronic sensors of choice for urine analysis and dental color matching applications. They allow medical professionals to automate analyses that used to rely on human judgments. Prior to optoelectronic sensors, urine analysis involved dipping a test strip into a specimen and trying to match the resulting color to a chart; dental color matching consisted basically of eyeballing color strips.
The combination of small size, sophisticated functionality, solid-state robustness, and low-power operation makes integrated optoelectronic sensors a natural choice in medical equipment design. The ability to create smaller, portable, noninvasive test equipment that provides quick, accurate results has led to the development of pulse oximeters, personal heart-rate monitors, and blood glucose meters. Integrated optoelectronic sensors have provided medical professionals with a quick, accurate procedure for analyzing urine specimens, as well as helping eliminate the need to look at color strips in dental color matching.
Optical Sensors in Pulse Oximetry
|
|
Pulse oximetry is a state-of-the-art noninvasive method for determining the percentage of hemoglobin (Hb) saturated with oxygen, an important measurement when administering anesthesia, determining the effectiveness of the respiratory system, or diagnosing various illnesses, such as pneumonia, pleurisy, and asthma.
Hemoglobin that is carrying oxygen (oxy-hemoglobin) absorbs light in the IR region of the spectrum; hemoglobin that isn't carrying oxygen (deoxy-hemoglobin) absorbs visible red light.
In pulse oximetry, a clip containing 2 LEDs and the light sensor is placed on the patient's finger (see Figure 1) or earlobe. One LED emits red light (600–700 nm) and the other emits light in the near IR (800–940 nm) region. The clip is connected by a cable to a microprocessor unit. The LEDs are rapidly and sequentially pulsed, and the detector is synchronized to capture the light from each LED as it is transmitted through the tissue. Backgrounds such as fluid, tissue, and bone are factored out of the measurement by monitoring the steady-state absorption from bone, tissue, venous blood, and arterial blood. During an arterial pulse there is an increase in blood volume, and this time-varying component is used to calculate the absorption of oxy- and deoxy-hemoglobin.
A photodiode has been the light sensor of choice in the past but there is growing interest in using either a light-to-voltage or light-to-frequency converter. When using a photodiode, considerable effort is placed into shielding it from noise. A light-to-voltage converter, such as the TAOS TSL257 with its integrated transimpedance amplifier, eliminates the need for this additional shielding. The light-to-frequency converter is an attractive choice because its output is digital rather than analog and therefore can interface directly to a microcontroller. It also can make measurements with resolution to 16 bits. The TAOS TSL260R, TSL261R, TSL262R, and TSL267 IR light-to-voltage converters and the TSL235R light-to-frequency converter are currently used in pulse-oximeter systems, and personal heart-rate monitors.
|
|
Integrated Color Sensors in Blood Glucose Meters
|
|
Most diabetics test their blood sugar level at least three times a day. Accurate and reliable results are top priorities when a diabetic chooses which blood glucose meter to use. Other factors considered are size and weight, cost of the meter, cost of the test strips, ease of use, and the minimum sample size required. Fingertips provide an ample supply of blood for testing, but hurt more than other parts of the body when poked. A meter that lets you test with a smaller quantity allows the sample to be taken from a less sensitive place such as the arm or thigh.
Of the two types of test methods used in meters today—electrochemical and light reflectance—we'll focus our discussion on the light-reflectance method. With this method, the blood sample reacts with a substance on a test strip so either there's a color change based on blood glucose content or it will exhibit certain properties when illuminated by a specific wavelength of light.
In meters using the light-reflectance method, the test strip is illuminated by a light source in the meter, usually an LED emitting in the visible range. The intensity of the light reflected back from the test strip is read by an optical detector, amplified, and converted before being fed to a microcontroller for processing. Great care is taken to limit the amount of ambient light seen by the detector, since any ambient light is considered noise and reduces the meter's accuracy.
The desired measurement depends on how the test strip's chemistry is designed to react with the blood sample. You might want the reflectance of a particular wavelength of light, which can be achieved by either limiting the light source to only that wavelength or by filtering the sensor to see only the wavelength of interest. There are advantages and disadvantages to both of these approaches. Limiting the wavelength means that more is spent on the LEDs to get a particular wavelength output, but it allows you to use a general-purpose detector. Filtering the sensor lets you use a less expensive light source and spend more on a filtered detector, such as the TSLR257, TSLG257, and TSLB257 from TAOS, which are light-to-voltage converters with integrated red, green, or blue filters, respectively.
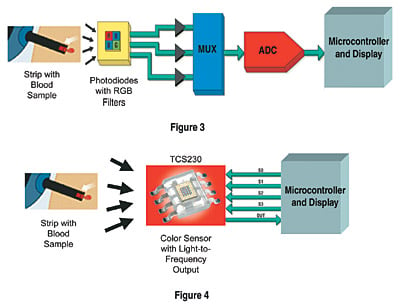
If you require spectral information from the strip, the approach is to use LEDs tuned for specific wavelengths with tight tolerances. The drawback is that the LEDs may be more costly and there must be a separate LED for each wavelength of interest. If you want to measure a change of color in the strip, then you can measure the intensity of one or all of its tri-stimulus RGB color components. If only one color component is needed, then a light-to-voltage converter with an integrated color filter for red, green, or blue, respectively, would be best. In most cases, it is desirable to measure the intensity of all three RGB components. Traditionally this has been done using photodiodes with RGB filters and discrete components (see Figure 3).
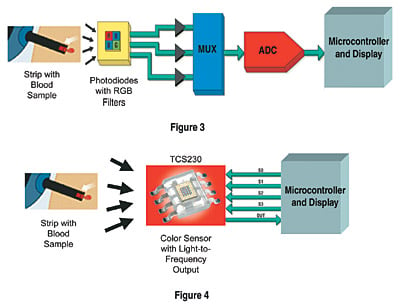
Figures 3 and 4. This illustrates how the choice of color sensors can affect the overall design of a blood glucose meter. The first approach (Figure 3) uses individual photodiodes with red, green, and blue filters, respectively. The color-filtered photodiode outputs are fed to a multiplexer for selection of the red, green, or blue light-intensity data. These data are converted from analog to digital format and sent to a microcontroller for processing. The second approach (Figure 4) uses the TAOS TCS230, which converts light intensity directly to a pulse train with a frequency proportional to the intensity of the red, green, and blue components. The output of the TCS230 can be fed directly to a microcontroller, eliminating the need for external amplifiers, multiplexers, and A/D converters.
|
The color-filtered photodiode outputs are fed to a multiplexer for selection of the red, green, or blue light-intensity data. These data are converted from analog to digital and sent to a microcontroller. A next-generation color sensor that converts light intensity directly to a pulse train with a frequency proportional to the intensity of the red, green, and blue components is now available from TAOS. The output of the TCS230 can be fed directly to a microcontroller, eliminating the need for external amplifiers, multiplexers, and A/D converters (see Figure 4).
|
|